In building a foundation for overall health, we can’t overlook the importance of behavioral health. Sadly, there’s been a longstanding gap between the attention given to behavioral healthcare (BH) and physical healthcare. The good news is that bridging this gap is gaining bipartisan support in Congress.
Significant changes will likely be made to mental health parity in the near future—possibly even next year. These changes aim to remedy the imbalances in how health plans cover behavioral health treatment compared to physical health treatment.
I understand the hesitation among health plan leaders to wait and see the unfolding developments. However, being proactive now is a ‘no regret’ approach that readies health plans for compliance and strengthens their behavioral health services. This move can expand their market share, especially as the demand for behavioral health services continues to rise.
Health plans can manage costs and realize a more significant return on investment by improving access to BH, reducing wait times, and delivering higher-quality comprehensive care.
Now is the opportune moment to craft and implement a strategic plan. Change is on the horizon, and being prepared positions us for a healthier and more balanced future.
Behavioral health parity and where it’s fallen short
The MHPAEA is an evolving body of legislation tracing its roots back to the first federal legislation in 1996 under the Mental Health Parity Act. At the time, it was the first U.S. legislation to establish that large-group health plans couldn’t place annual or lifetime dollar limits on mental health benefits that were less favorable than limits imposed on medical benefits—a groundbreaking step.
Over the past 28 years, this legislation has undergone significant expansions:
- 2008: The Mental Health Parity Act evolves, now encompassing protections for substance use disorder (SUD) treatments. This transformation leads to its new title, the Mental Health Parity and Addiction Equity Act.
- 2010: The Affordable Care Act extends MHPAEA requirements to individual health insurance coverage and regulates small group health plans, declaring mental health treatment and SUD essential health benefits.
- 2013: Additional layers of protection are added, specifying that parity requirements extend to financial aspects, quantitative treatment limitations (QTLs), and non-quantitative treatment limitations (NQTLs).
- 2021: A more refined focus emerges, including specific analytical requirements for NQTLs related to mental health and SUD benefits. This mandates a comparative analysis of the design and application of these limitations compared to medical health benefits. Furthermore, this analysis must be readily available to regulatory agencies upon request.
Where has this evolution left behavioral health benefits?
Even when a health plan extends behavioral health benefits and claims to have a sufficient number of providers within members’ zip codes, many still face challenges in accessing treatment.
Often, individuals discover a lack of local providers who accept their insurance, contend with long wait times, or can’t get appointments. Ghost networks further compound these issues, leading many to seek care from out-of-network providers.
- Behavioral healthcare is accessed through an out-of-network provider five times more frequently than a primary care visit
- For minors, the likelihood increases to ten times
There are persistent gaps in accessing quality behavioral healthcare. The proposed MHPAEA regulations aim to address some of these challenges and pave the way for improved access to essential mental health services.
Proposed changes to the MHPAEA
Let’s briefly outline the three key provisions of the proposed changes to the MHPAEA.
Comprehensive coverage mandate
Plans must offer meaningful benefits to mental health and substance use disorder. If a plan treats a specific condition in one benefit classification, it must offer treatment in all six classifications, such as inpatient/in-network, inpatient/out-of-network, outpatient/in-network, outpatient/out-of-network, prescription drugs, and emergency care. For example, if a plan offers in-network mental healthcare, it needs to meet all the comparative analysis requirements, showing that its provision of and access to mental healthcare in-network is in parity with its provision of medical and surgical benefits.
Expanded protection
Eating disorders and autism spectrum disorders are now recognized as mental health conditions, gaining protection under the MHPAEA. So, health plans are mandated to cover treatments for these conditions. As mentioned above, if a plan covers these treatments in one benefit classification, it has to cover them in all six.
Data-driven action
Data must be gathered and assessed, and plans must take action based on the outcomes data. This means plans must address any “material differences” the outcomes data shows in members’ access to mental health and substance use disorder benefits compared to medical and surgical benefits.
These actions must be thoroughly documented in the comparative analysis of non-quantitative treatment limitations (NQLT). The goal is to ensure transparency and tangible improvements in access to mental health and substance use disorder benefits.
How Spring Health can act as a compliance partner
The proposed changes offer hope for improved access to quality behavioral healthcare in-network and in a timely manner.
It’s worth noting that while these regulations aim for positive shifts, they come with complexities and bureaucracy. The intricate nature of the rules, coupled with the yet-to-be-determined specifics and timing, adds an element of uncertainty. The final shape and implications of these regulations remain unknown.
Nevertheless, the days of compliance in name only are about to end. Whether these changes are perceived as a measured step or an ambitious leap, health plans are heading toward a new era of more stringent compliance in behavioral health. Preparing for these changes is pivotal as we move toward a landscape where adherence to regulations will be more rigorous and impactful.
Now is the time to start having compliance conversations
Segal’s recent webinar highlighted the evolving landscape of MHPAEA enforcement amid regulatory uncertainty. They suggested health plans and plan sponsors must engage with vendors proactively to navigate this terrain. Communication with vendors becomes crucial in assessing their capacity to support compliance efforts, including providing proposed data and claims reporting.
Spring Health is well-positioned to collaborate with health plans in addressing data collection, access, and outcome gaps. Our expertise aligns with the key components of the new regulations, and we’re committed to partnering with health plans by:
- Providing meaningful and accessible behavioral health benefits to assist the plan's parity with medical benefits
- Collecting and providing documentation and evidence to allow the plan to meet regulatory requirements
- Extending support for the inclusion of treatment for eating disorders and autism spectrum disorders as recognized mental health conditions covered by the MHPAEA.
Let’s dig into more detail.
Data collection and evaluation
The proposed rules outline detailed requirements for the non-quantitative comparative analysis (NQTL), emphasizing the importance of specific data and information. These include:
- Network adequacy metrics
- In-network versus out-of-network utilization rates
Regulators have struggled to establish NQTL parity because assessment standards are subjective, so the new regulations greatly emphasize data. Plans must have valid data sources and analytical tools to evaluate access and outcome data.
This emphasis on data aims to bring objectivity and transparency to the assessment process, facilitating a more comprehensive understanding of behavioral health benefits within health plans.
Network adequacy metrics
Spring Health has the internal capability to build and adapt a comprehensive provider network. Our approach involves leveraging member location data to identify network gaps and subsequently building and optimizing the network to cater to those specific needs.
To enhance network adequacy, we offer:
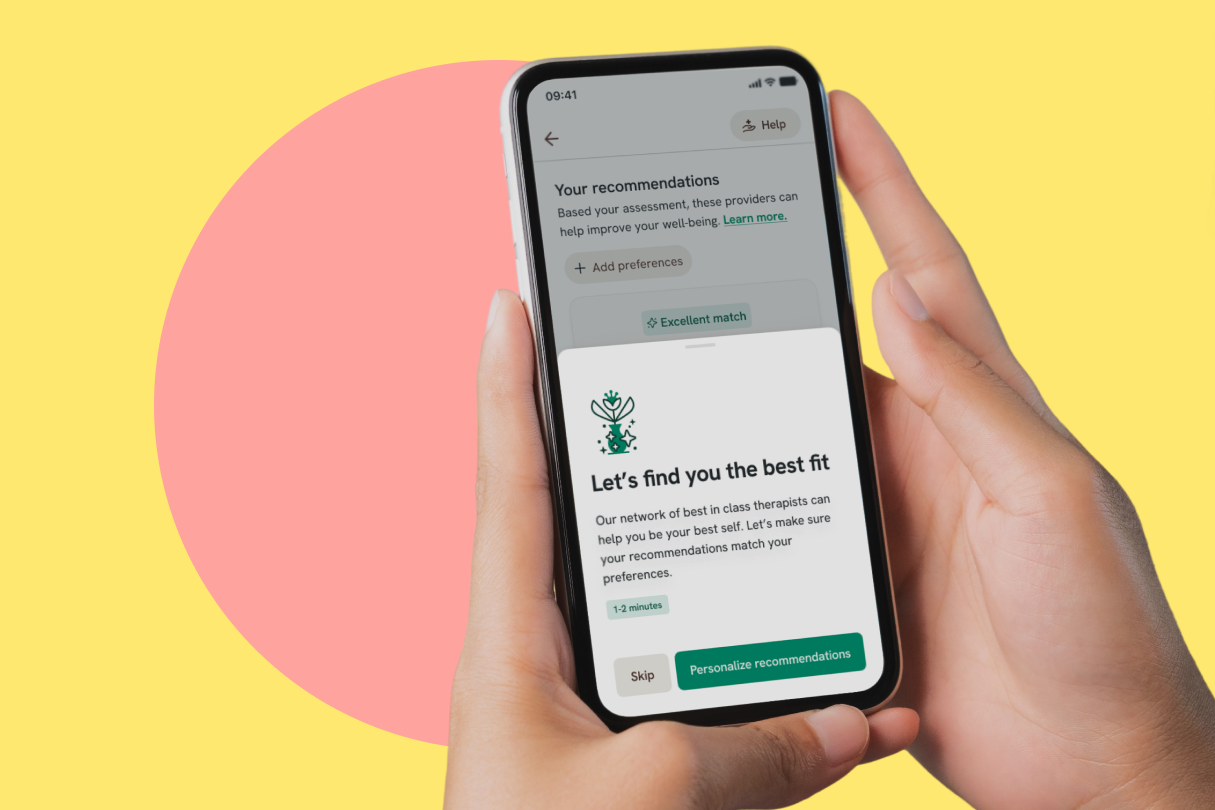
- Personalized provider recommendations, a rigorous provider hiring process, and ongoing provider training
- Better access to care across all populations due to our diverse provider network and less than two days for an appointment across all states
- Information to enrollees on the availability of in-network providers, including real-time availability, direct scheduling, and referral concierge services to other care outside of Spring Health
In-network utilization rates
Spring Health takes a proactive stance on compliance by collecting and assessing standard member-level utilization data. Our data collection extends to members’ proximity to providers, time to appointment for new patients, and practitioner-to-enrollee ratios.
To drive utilization, we go beyond data metrics. We offer a personalized treatment approach through care navigation, coordination, and integration. This ensures a seamless experience for all parties involved—making both inbound and outbound referrals effortless for the plan, providers, and members.
New additions to covered mental health conditions
Under the proposed rules, Spring Health is poised to address compliance by extending our support to encompass eating disorders and autism spectrum disorders within the regulatory framework of the MHPAEA.
Our solutions include:
- Comprehensive eating disorder support
- Mental health support for individuals on the autism spectrum, including providers who specialize in this area
Shifting from a compliance mindset to an opportunity mindset
Taking a proactive approach to the imminent changes in behavioral health parity is a strategic move for health plans. This proactive stance serves three crucial areas:
- Early preparation for behavioral health parity compliance. By getting ahead of the curve, health plans can proactively prepare for compliance with behavioral health parity regulations. This positions them to adapt to the evolving regulatory landscape seamlessly.
- Enhanced return on investment. A proactive approach ensures compliance and presents an opportunity to improve ROI. This can be achieved by driving better access to behavioral healthcare and optimizing outcomes for plan members. One likely outcome of the new regulations is greater access to care at higher unit costs to comply with NQTLs. Given that, it will be critical to ensure the increased spend on behavioral health actually reduces the total cost of care.
- Addressing member needs. Anticipating and aligning with plan members’ behavioral health needs is a key aspect of a proactive strategy. This ensures health plans are responsive to the evolving demands in the healthcare landscape.
Now, more than ever, is the time for health plans to ensure compliance with proposed rules and enhance member access to comprehensive, clinically-validated behavioral healthcare.
Explore innovative solutions to escalating healthcare costs and a surge in demand for behavioral healthcare, and discover how Spring Health is challenging the myth that affordability and access are incompatible.












_405x405.png)