The need for high-quality behavioral healthcare is profound, and the existing system is broken. It’s internally fragmented, difficult to access, challenging to navigate, and regularly ineffective, leading to unnecessary medical spend.
Simply put, individuals who need quality care are not getting it. Instead, they’re experiencing:
- Long wait times: the average national wait time for a behavioral health appointment is 48 days, and if you're looking for a specialist in a particular area or with specific attributes, wait times can stretch into months
- Frustration: 42% of health plan members find the behavioral health experience frustrating
- Inefficient care: only 18% of psychiatrists and 11% of psychologists in the U.S. routinely use measurement-based care to monitor treatment response
We have a powerful opportunity to enhance behavioral healthcare to better serve the needs of individuals seeking care while also increasing the cost-effectiveness of these systems.
Key tenets of a patient-centered, integrated continuum of care
Six overarching pillars of care are necessary for improving access, engagement, and outcomes. Effective, quality care is:
- Easy to enter: When individuals first access this system, the entry point connects them to a wide array of high-quality, integrated care modalities for all levels of acuity, across a wide range of behavioral health conditions. These may include digital content, coaching, therapy, and/or medication management. Individuals are also precision-matched with the right provider.
- Integrated: Care is not designed to be one-size-fits-all. Instead, it’s holistic and integrated with physical healthcare to meet the unique needs of each individual based on their journey.
- Supported by care navigation: Each individual engaged in care is partnered with a dedicated Care Navigator, who is a licensed master’s level clinician. They work with the patient longitudinally to remove barriers and motivate them to stay in care.
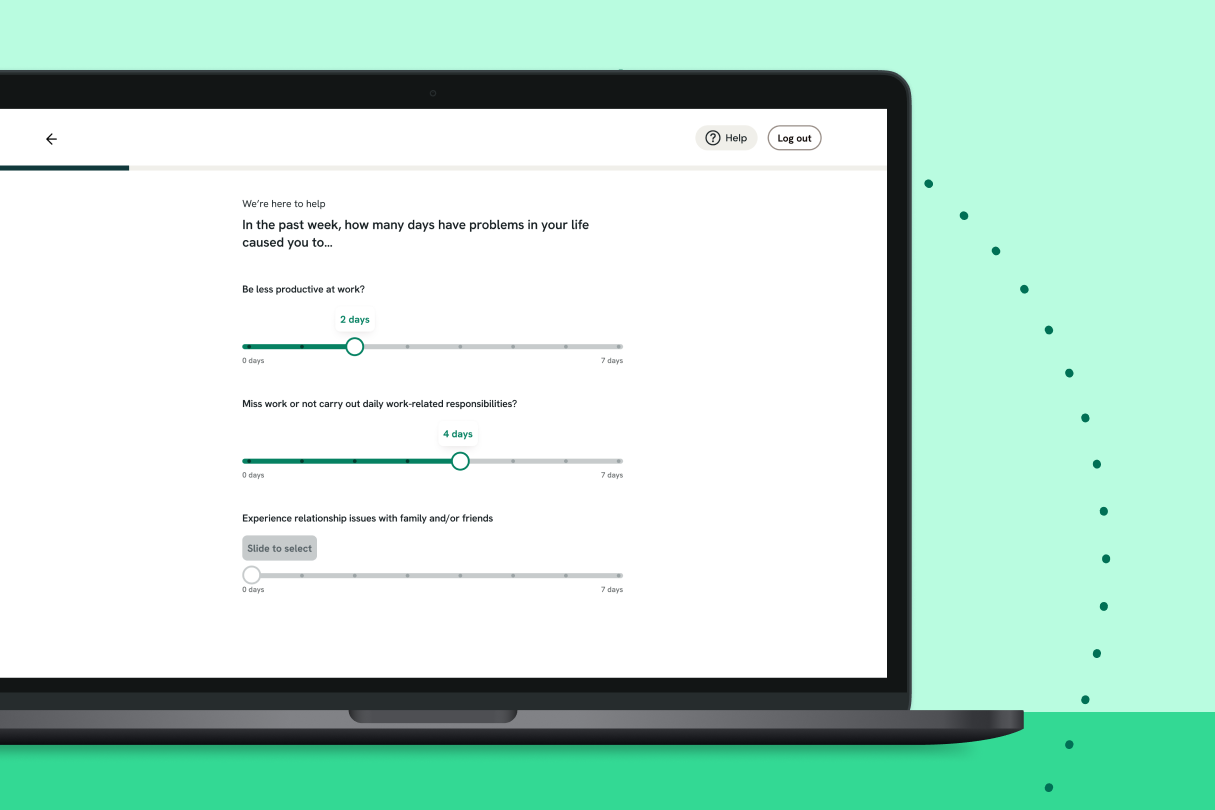
- Data-driven: Measurement-based, outcome-oriented care should be the standard. Behavioral healthcare will remain stagnant without leveraging data to improve care delivery, behavioral health treatment will remain stagnant. You can’t improve what you can’t measure.
- Utilizing technology: Support providers with technology and tools that allow them to focus on providing care while spending less time on administrative tasks.
- Addressing the social determinants of health: Optimal behavioral health can’t be achieved without ensuring that essential needs are met. In particular, addressing social, economic, and physical needs should be integrated into behavioral health support, as one cannot thrive without the other.
Next, let’s explore the granular details of each pillar.
Centering the patient experience
It’s essential to build our entire foundation on what the experience of getting behavioral healthcare feels like to the patient or member.
In other words, we must truly put the individual at the center and then build a system that works for their needs and feels good to use. This starts with making care easy to enter.
Making entry easy, legible, and simple to navigate
Currently, entry into behavioral health care is chaotic and messy. Individuals aren’t sure where to start or how to enter care.
When they do, they often experience long wait times and trial-and-error treatments. Many bounce around to different, disconnected providers as they struggle to figure out what care modalities will actually be effective for them.
It doesn’t have to be this way. Everyone who is struggling deserves fast access to effective and efficient behavioral healthcare.
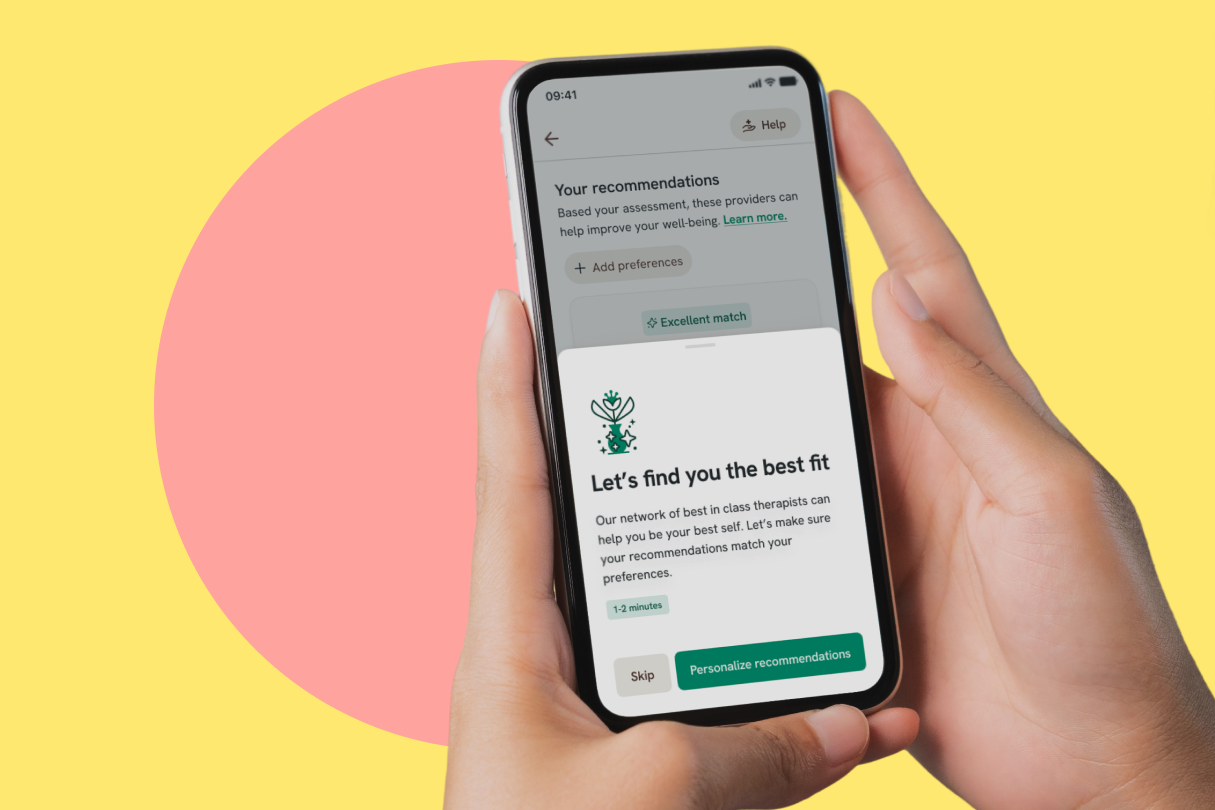
Here’s what that looks like: members are stratified into the right level of care the first time they seek entry into a behavioral healthcare network, and that network is easy to navigate. For example, an individual with low-level acuity can enter the same front door for support as someone with higher acuity needs.
In this model, the individual isn’t responsible for figuring out their care level. Instead, the right level of resources, including digital CBT, coaching, therapy, or medication management, is immediately available to members. Treatment will likely include some combination of modalities.
However, we can’t fix the problem by adding more entry points. Individuals already contend with ghost networks, constrained access, and dubious clinical quality.
We need smarter entry points to connect people quickly with the right care the first time—not an increasingly frustrating game of “choose-your-own-adventure.”
Improving the access problem
According to the Association for Health Insurance Plans’ data, two-thirds of health plan members who seek care have to wait at least one month to get an appointment, and one-third of members seeking care end up waiting more than two months.
Improving this critical area doesn’t just mean giving health plan members a long list of providers. It’s important to ensure that individuals can get an appointment with a provider accepting new patients, has a specialty that suits their needs and has matching availability.
Here are two things to look for in a provider network to ensure a behavioral health solution can help members access the care they need quickly:
- Can the network prove a low average time to first and third appointments? Many solutions have a low average time to first appointment with high wait times for a third appointment. This is the best network capacity indicator—much more than a network’s size.
- Can the network demonstrate that these averages have remained sustainable over time?
The last thing people who are dealing with behavioral health issues need is a fight to get into high-quality care. That should be the easy part.
By leveraging technology, we can quickly connect people with the right care the first time.
Ensuring quality of care
Getting an initial appointment with a behavioral healthcare provider doesn’t necessarily indicate that an individual is on the path to recovery.
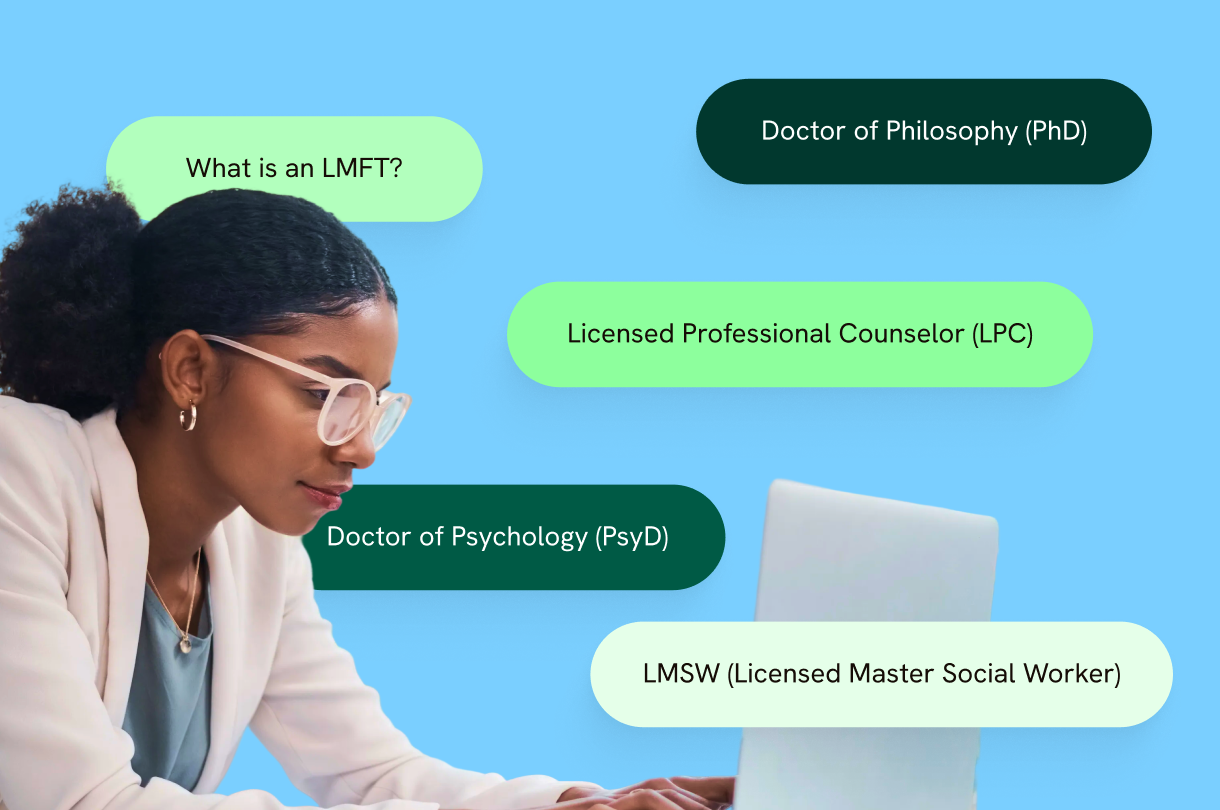
When someone seeks care, scrolling through a list of uncurated provider options isn’t the most efficient way to find the right provider. How could they know if they need an LCSW, a psychologist, or a psychiatrist? Or a provider’s success rate in getting their patients into remission?
It’s now possible to use machine learning tools to intake patient data—in the form of standard clinical scales, member demographics, type of treatment, the provider’s cultural competency, social determinants of health, and member preferences—and run those data points through machine learning models. These models can be used to match an individual with the best provider for their needs.
When this is done right, trial-and-error care is replaced with precision, pairing patients with the ideal provider and treatment modalities—ultimately, getting people into remission more quickly.
High-touch patient navigation
For individuals engaging in care, having a licensed, clinically experienced professional available to guide them through getting care increases the likelihood that they’ll stay in care.
Health plan members should be able to contact their Care Navigator anytime to get recommendations and referrals, crisis intervention, and anti-stigma interventions.
When someone needs a higher level of care, it’s helpful to have a referral concierge in place to connect them with the appropriate level of care. For example, an individual may need intensive inpatient or outpatient care.
Integrating technology and digital solutions
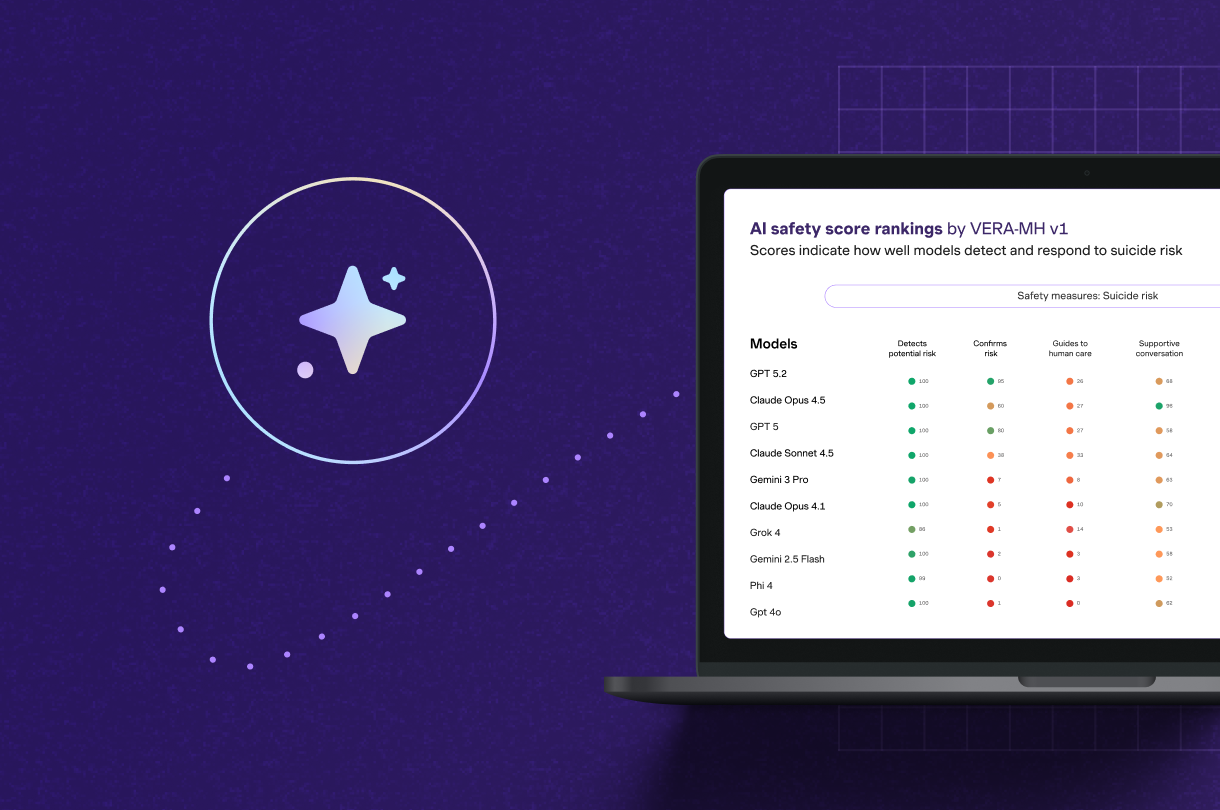
New and evolving technology solutions can help providers implement measurement-based care, driving better outcomes and faster patient remission. For example:
- Candela by Spring Health is a system used to measure and identify high-quality care at the provider level—and align incentive payments to compensate providers for better outcomes.
- Compass by Spring Health is an electronic health records platform that allows easy collaboration with other patient treatment team members. This includes the individual’s primary care physician, therapist, medication manager, and care navigator.
- Spring Health’s precision provider matching gives individuals access to the industry’s most diverse provider network. Fifty percent identify as BIPOC and speak 50+ languages.
The different providers on the patient’s team can focus on using data to improve the care plan and treatment outcomes. They can easily view what’s working and not working for the patient, getting them better, faster treatment.
Once a provider has the right tools, bi-directional data sharing between the behavioral health provider and the member’s primary care physician becomes seamless.
Addressing the social determinants of health
Some aspects of employee health may fly under the radar in a workplace environment, including non-medical factors that deeply influence physical health, mental health, and quality of life. Forty-five percent of adults in the U.S. have at least one unmet need, such as food insecurity or loneliness.
Even individuals who work full-time may struggle with food insecurity, stable housing, and childcare.
Addressing these employee needs in the workplace might entail integrating vetted community resources and organization-sponsored benefits within a comprehensive behavioral health solution.
As part of an employee’s initial mental health assessment, as they engage with the solution, they might be screened and connected with food and housing services and specialized care, like fertility support and disability management.
The individual could also be paired with advocates, such as social workers, who can help them navigate complex eligibility requirements for community programs.
A behavioral healthcare thought experiment
What if we could wave a magic wand to fix behavioral healthcare? How would we wield this power?
First, we’d remove all the barriers to high-quality, behavioral healthcare for everyone, which requires reimagining the traditional care delivery model. The hopeful part of this thought experiment is that with new tools and technologies, we’re already on the road to making this a reality.
We can sum up what we think needs to change to bring this thought experiment to reality with these four things:
- Measuring quality of care based on patient outcomes and recovery rates
- Getting people access to the right care when they need it, with an easy entry to care
- New behavioral health infrastructure where people can utilize provider services anywhere in the country
- Ensuring that non-medical needs such as food, housing, and social support are included as part of a holistic understanding of behavioral health
Structurally, one of the biggest artificial impediments to connecting people with high-quality providers is the state-based, legacy licensing system for behavioral healthcare providers.
Quality behavioral health treatment is hamstrung by state-by-state licensing requirements for highly trained clinicians. Regardless of state licensure, delivering behavioral health across state lines is a highly effective way to drive access. This should be the standard, not the exception.
Explore innovative solutions to behavioral healthcare treatment and discover how Spring Health is challenging the myth that affordability and access are incompatible.











_405x405.png)