Access to behavioral healthcare is an essential component of comprehensive and high-quality care, and plays a fundamental role in determining overall health outcomes. Neglecting behavioral health concerns or erecting barriers to care can have severe ramifications for health insurance plans and their members.
While barriers to behavioral healthcare are high for many people, historically marginalized populations face even greater obstacles to securing treatment due to bias and structural inequality.
In other words, barriers to care are not distributed equally. This is, first and foremost, a moral issue. Health plans have an opportunity to address a historically fractured system that continues to impact millions of people today, and many are seizing it.
At the same time, untreated behavioral health issues raise the amount health plans are spending, exacerbating existing health issues and highlighting the crucial need for health plans to address this inequitable dynamic.
How access correlates with overall health outcomes
Overall health and well-being are deeply intertwined with behavioral health, and even more specifically, mental health.
As an example, take two people with the same health issue, diabetes. The person with an untreated mental health illness, in tandem with a physical health issue, will spend a significantly higher annual amount on medical care.
For underserved communities, unequal barriers to accessing behavioral healthcare equates to higher costs for that population. Of course, the human cost of suffering is equally significant, with an estimated 117,00 premature deaths amongst racial, indigenous, and ethnic minorities in the U.S. during a four-year period.
Barriers to care for marginalized groups exist across the healthcare spectrum
Marginalized groups face systemic inequalities with accessing healthcare overall—in how they are diagnosed and treated for behavioral health issues, and in terms of clinical outcomes for all forms of healthcare.
The root causes of these inequalities are complex and deeply rooted in systemic factors that arise from historical conditions, including structural racism, provider discrimination, stigma, misdiagnosis and underdiagnosis, and lack of insurance, all of which are informed by the social determinants of health (SDOH).
Social determinants of health include:
- Economic conditions
- Access to education and quality education
- Availability of healthcare
- Neighborhood and built environment factors
- Social and community context
The social conditions in which people live impact their health outcomes, and can contribute to barriers keeping people from accessing services that might improve those outcomes.
Barriers to health equity aren’t theoretical. Here are some real world examples of how health inequities play out in the realm of healthcare:
- Racial disparities in diagnosing and treating depression
- Gender biases in patient care
- Barriers to addiction treatment due to racial bias
- Racial disparities in maternal health outcomes
- Barriers to mental health treatment for LGBTQIA+ individuals
- Disparities in outcomes for pediatric transplants
This is only a small sample of research outlining barriers to care for underserved communities. It’s also helpful to understand how systemic problems and biases affect the daily lives of people seeking care for behavioral health issues.
What barriers to behavioral care look like on an individual level
A 2016 study from the American Sociological Association paints a grim picture of the reality marginalized individuals face when they try to access behavioral care.
Voice actors recorded messages seeking care from therapists, which were then used to leave voicemails for multiple therapists. The voice actors were assigned names and speech patterns coded as Black or White and working or middle class.
All callers had the same insurance, yet the Black working class man received only one call back offering care after 80 messages were left for different therapists—while the White middle class caller had 20% of her calls returned.
Ultimately, the working class received return calls at significantly lower rates than middle class callers, with Black working class callers least likely to receive a call back.
If someone from a marginalized community struggles with a mental health illness or issue and calls even ten therapists without receiving a single return call, that’s a huge initial hurdle.
And if the individual perseveres and finally does find a therapist, but the therapist doesn’t understand their lived experience, it’s less likely they can provide quality care.
This serves as only one example of how people from underserved communities, which can include intersections of racial, ethnic, gender, sexual orientation, economic, cultural, and/or linguistic social identities, encounter unequal access to healthcare.
Compounding barriers to care
Dealing with bias in addition to depression, anxiety, or any other well-being challenge further compounds the barriers to accessing care.
It’s important to acknowledge that people frequently don’t fit into a single category or identity. Many inhabit multiple marginalized identities simultaneously.
The 2016 study is a good example. Black callers who were also working class were much less likely to be called back than Black, middle class callers.
Access to behavioral healthcare lowers medical spend
An assessment done by Altarum showed that racial health disparities cost around $7.7 billion in excess medical spending and lost productivity in just one state, with an overall cost of $278 billion over four years in the U.S.
When behavioral health is left unaddressed, health plans experience higher expenditures. Removing barriers to care is not only ethical, but also better for financial ROI. This is a rare case where doing what’s right and what’s cost-effective are aligned—and the solution democratizes access to behavioral health treatment.
How Spring Health is democratizing access to care
Let’s go back to the voice actor example we covered earlier, which represents a broader issue: the initial barrier to accessing care frequently prevents people in marginalized populations from making it through the door.
It needs to be as easy and painless as possible for someone dealing with behavioral health issues to make an appointment. No one suffering from depression should have to call 80 providers to get one call back.
Spring Health partners with health plans and employers worldwide to offer high-quality, comprehensive behavioral healthcare that’s precise, personal, and proven.
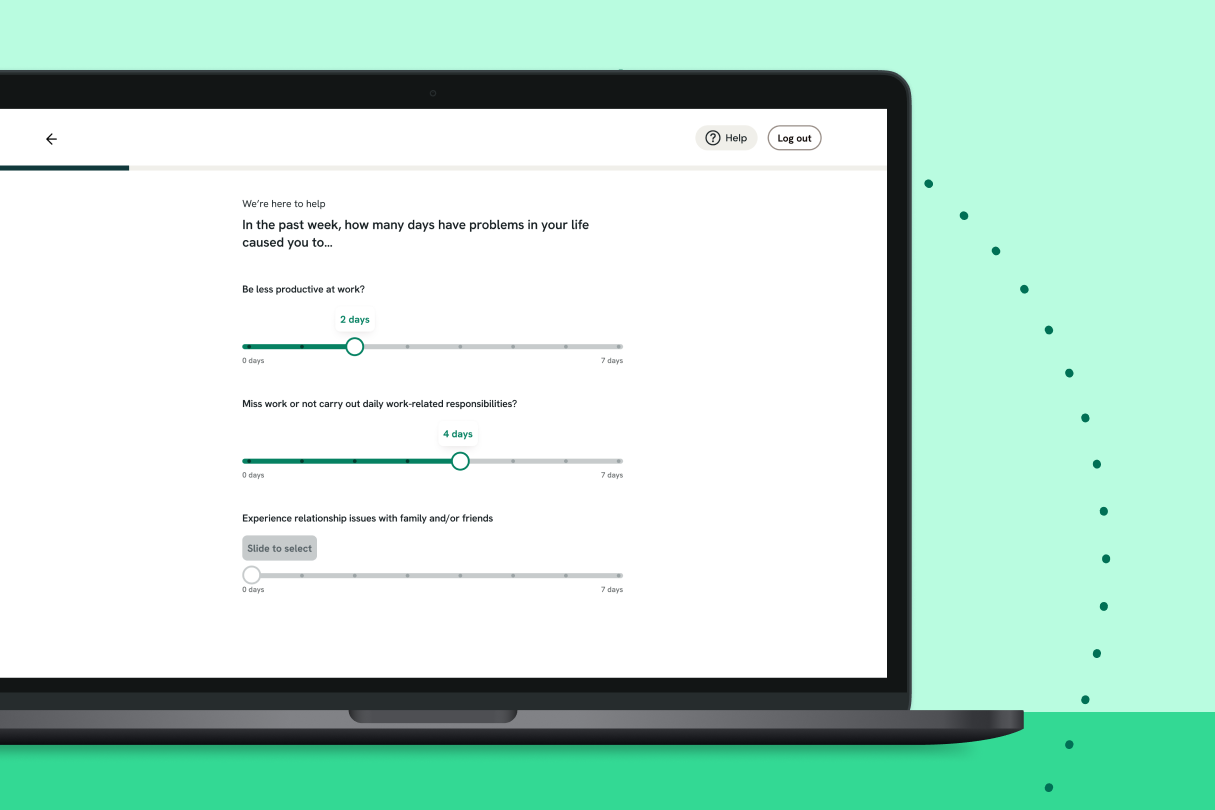
A member’s journey with Spring Health begins with a short, clinically-validated assessment, which screens for over 12 different clinical issues. During the assessment, our AI-based technology uses millions of data points to create a personalized plan for the member.
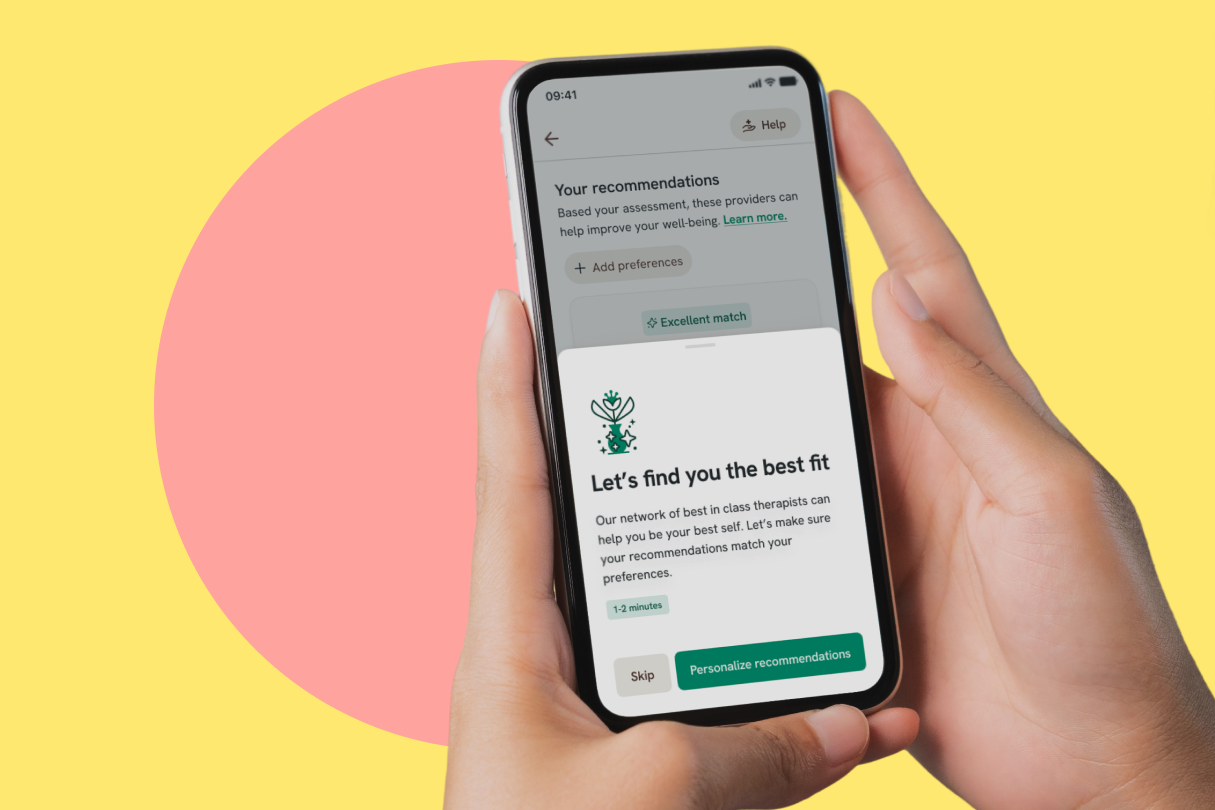
If therapy or coaching is part of that plan, members are matched with a provider who has expertise in their specific needs—and they can schedule their initial appointment in less than two days. There’s no waiting for a call back or chance for bias to keep anyone from care.
We make it easy for everyone to access care. Our providers are available during the day, and on evenings and weekends to ensure therapy and coaching fit into the member’s schedule—not the other way around.
Therapeutic alliance is key for breaking down barriers to care
Matching individuals with the correct type of care is the first part of the equation to help eliminate that initial barrier to access. Next, they need to form a bond with their provider, often referred to as therapeutic alliance.
Studies have shown that establishing a therapeutic alliance improves clinical outcomes. However, building this alliance can be more challenging with underserved groups for two reasons.
First of all, there’s a shortage of providers from disenfranchised communities. When someone seeks care from a therapist who isn’t part of their community, they’re more likely to encounter racism, transphobia, and other forms of bias.
Additionally, establishing a therapeutic alliance is facilitated when the provider possesses a comprehensive understanding of the client’s lived experience.
Spring Health offers a diverse provider network, so members can find a therapist or coach who looks and sounds like them and has a similar background. Within the Spring Health platform, members can filter providers based on language, ethnicity, race, sexual identity, gender identity, or other characteristics.
Each member has access to a dedicated Care Navigator, who is a master’s level licensed clinician and provides guidance and personalized support. If the member has unique overlapping identities, a Care Navigator can help them find a therapist who fits their specific needs.
Our diverse provider network offers stronger therapeutic alliance, better member satisfaction, and better clinical outcomes—all of which mean lower medical spend over time.
Data driven for better clinical outcomes
Spring Health uses clinically validated technology, called Precision Mental Healthcare, to pinpoint and deliver precisely what will work for each person—whether that's meditation, coaching, therapy, medication, or a combination of modalities.
Precision Mental Healthcare results in:
- 4 week recovery time, which is 8 weeks faster than average
- Measurement-based care
- Lower overall medical spend for better financial ROI
- Proven clinical outcomes
This translates into savings for health plans. We’re delivering 12% savings and lower medical spending over one year, which then compounds for those members who stay in care for years two and three.
Health insurance plans have an opportunity to do something rare: eliminate barriers to behavioral healthcare for individuals who have been widely discriminated against, and lower medical spending at the same time. This really is a win for everyone.
Discover how the leading behavioral health solution is delivering validated clinical improvements for members and financial savings for partners.












_405x405.png)